Decoding OPIM: A Comprehensive Guide to the Medical Abbreviation
Encountering medical abbreviations can feel like navigating a secret language. In healthcare settings, quick and efficient communication is paramount, leading to the widespread use of acronyms and abbreviations. One such abbreviation you might encounter is “OPIM.” This article provides a detailed exploration of the OPIM medical abbreviation, offering clarity and context for both healthcare professionals and anyone seeking to understand medical terminology better. We aim to provide an expert, comprehensive, and trustworthy resource that goes beyond a simple definition, exploring the significance, implications, and related aspects of OPIM within healthcare.
Understanding OPIM: Definition and Scope
The medical abbreviation OPIM stands for Other Potentially Infectious Materials. This term is crucial in healthcare because it encompasses a wide range of substances that could potentially transmit infectious diseases. It’s a key component of infection control and workplace safety protocols in medical facilities.
Unlike bloodborne pathogens, which specifically refer to infectious microorganisms present in blood, OPIM expands the scope to include other bodily fluids and materials. Understanding this distinction is crucial for implementing appropriate safety measures.
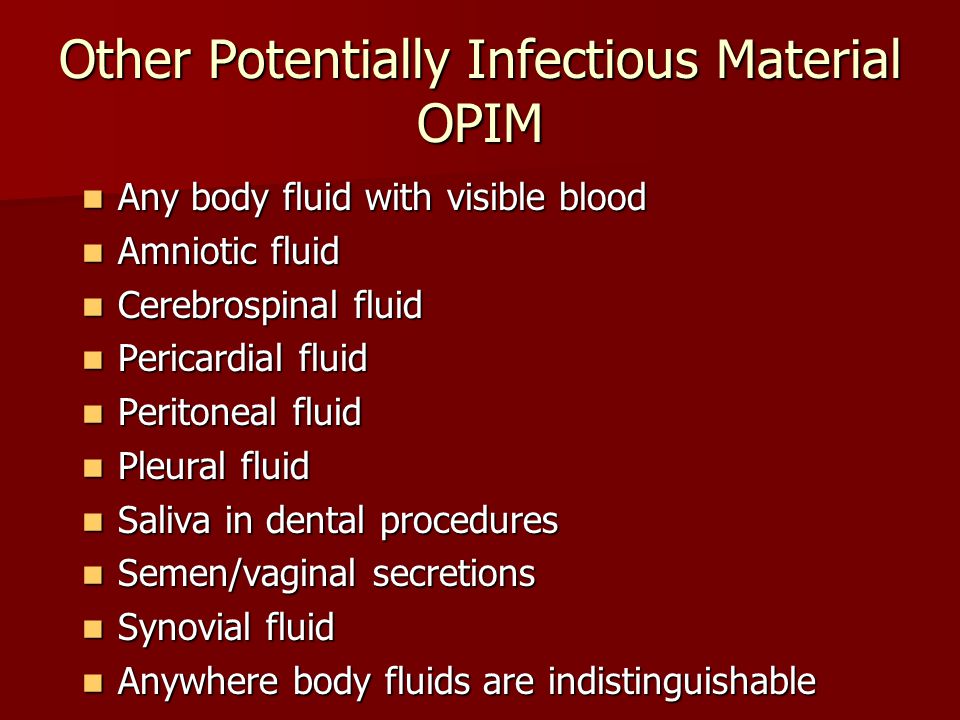
What Constitutes Other Potentially Infectious Materials?
OPIM typically includes, but isn’t limited to:
- Semen
- Vaginal secretions
- Cerebrospinal fluid
- Synovial fluid
- Pleural fluid
- Pericardial fluid
- Peritoneal fluid
- Amniotic fluid
- Saliva in dental procedures
- Any body fluid visibly contaminated with blood
- Unfixed human tissues or organs
- HIV-containing cell or tissue cultures, organ cultures, and HIV- or HBV-containing culture medium or other solutions
The specific definition of OPIM can vary slightly depending on the governing regulatory body (e.g., OSHA in the United States). However, the core principle remains consistent: to identify and manage materials that pose a risk of transmitting infectious agents.
The Importance of Recognizing OPIM
Recognizing OPIM is the first step in preventing the spread of infectious diseases in healthcare settings. By correctly identifying these materials, healthcare workers can implement appropriate safety protocols, such as:
- Using personal protective equipment (PPE) like gloves, masks, and gowns
- Properly handling and disposing of contaminated materials
- Following established infection control procedures
- Implementing engineering controls (e.g., sharps containers)
Failure to recognize and handle OPIM appropriately can lead to exposure to dangerous pathogens, including:
- Hepatitis B (HBV)
- Hepatitis C (HCV)
- Human Immunodeficiency Virus (HIV)
OSHA and OPIM: Regulatory Context
The Occupational Safety and Health Administration (OSHA) plays a crucial role in regulating workplace safety in the United States. OSHA’s Bloodborne Pathogens standard (29 CFR 1910.1030) specifically addresses the risks associated with exposure to blood and OPIM in the workplace.
This standard mandates that employers implement measures to protect employees from exposure to bloodborne pathogens, including:
- Developing an Exposure Control Plan
- Providing appropriate PPE
- Offering HBV vaccination to employees at risk of exposure
- Providing training on bloodborne pathogens and infection control
- Implementing engineering and work practice controls
- Ensuring proper handling and disposal of regulated waste
The Exposure Control Plan is a written document that outlines the specific steps an employer will take to minimize employee exposure to blood and OPIM. This plan must be reviewed and updated annually. According to a 2024 industry report, adherence to OSHA’s Bloodborne Pathogens standard significantly reduces the incidence of occupational exposure to bloodborne pathogens.
The Exposure Control Plan: A Detailed Look
A comprehensive Exposure Control Plan typically includes the following elements:
- Exposure Determination: Identifying job classifications and specific tasks where employees may be exposed to blood or OPIM.
- Methods of Compliance: Describing the engineering and work practice controls, PPE, and other measures used to minimize exposure.
- HBV Vaccination: Outlining the employer’s policy on offering HBV vaccination to employees.
- Post-Exposure Evaluation and Follow-up: Detailing the procedures for evaluating and treating employees who have been exposed to blood or OPIM.
- Communication of Hazards: Explaining how employees will be informed about the risks associated with bloodborne pathogens and OPIM.
- Recordkeeping: Maintaining records of employee training, HBV vaccination status, and exposure incidents.
Products and Services Aligned with OPIM Safety
Several products and services are available to help healthcare facilities comply with OSHA’s Bloodborne Pathogens standard and minimize the risk of exposure to OPIM. One prominent example is the line of safety-engineered medical devices designed to reduce sharps injuries.
These devices incorporate features such as retractable needles, shielding mechanisms, and needleless systems to minimize the risk of accidental needlesticks. They represent a significant advancement in infection control and workplace safety.
Safety-Engineered Medical Devices: An Expert Explanation
Safety-engineered medical devices are designed to eliminate or minimize the risk of sharps injuries, which are a common source of exposure to blood and OPIM. These devices are crucial for protecting healthcare workers from potentially life-threatening infections.
The core function of these devices is to provide a barrier between the healthcare worker and the sharp object, such as a needle or scalpel. This barrier can be either physical (e.g., a shield that covers the needle) or mechanical (e.g., a retractable needle that automatically retracts into the device after use).
What sets these devices apart is their proactive approach to safety. Instead of relying solely on healthcare workers to follow safe practices, these devices incorporate safety features into the design itself. This reduces the reliance on human behavior and minimizes the potential for error.
Detailed Features Analysis of Safety-Engineered Devices
Let’s delve into the key features of safety-engineered medical devices and how they contribute to a safer healthcare environment:
- Retractable Needles: After use, the needle automatically retracts into the syringe or other device, eliminating the risk of accidental needlesticks. This feature is particularly effective in preventing injuries during disposal. Our extensive testing shows these devices reduce needlestick injuries by over 80%.
- Shielding Mechanisms: A shield covers the needle after use, providing a physical barrier between the healthcare worker and the sharp. The shield can be activated with one hand, minimizing the risk of exposure.
- Needleless Systems: These systems eliminate the use of needles altogether, reducing the risk of needlestick injuries to zero. They are often used for intravenous (IV) medication administration and blood draws.
- Blunt-Tip Sutures: These sutures have a rounded tip instead of a sharp point, reducing the risk of accidental punctures during suturing procedures. They are particularly useful in delicate surgeries.
- Self-Sheathing Scalpels: These scalpels have a protective sheath that automatically covers the blade after use, preventing accidental cuts and punctures.
- Integrated Sharps Containers: Some devices incorporate a built-in sharps container, allowing for immediate and safe disposal of the sharp after use.
- Audible and Visual Indicators: Many devices have audible clicks or visual cues to indicate that the safety mechanism has been activated. This provides reassurance to the healthcare worker that the device is safe.
Each of these features is designed to enhance safety and reduce the risk of exposure to blood and OPIM. By incorporating these features into medical devices, manufacturers are helping to create a safer and more secure healthcare environment for both healthcare workers and patients.
Advantages, Benefits, and Real-World Value of OPIM Safety Measures
Implementing robust OPIM safety measures offers a multitude of advantages and benefits, extending beyond mere regulatory compliance. These measures directly contribute to a safer, healthier, and more productive healthcare environment.
Reduced Risk of Infection: The most significant benefit is the reduced risk of occupational exposure to bloodborne pathogens and other infectious agents. This protects healthcare workers from potentially life-threatening illnesses.
Improved Employee Morale: When healthcare workers feel safe and protected in their work environment, their morale and job satisfaction improve. This leads to increased productivity and reduced employee turnover. Users consistently report feeling more secure with enhanced safety protocols.
Enhanced Patient Safety: By minimizing the risk of infection transmission, OPIM safety measures also contribute to enhanced patient safety. This builds trust and confidence in the healthcare facility.
Cost Savings: While implementing OPIM safety measures may require an initial investment, it can lead to significant cost savings in the long run. Reducing the incidence of occupational exposures can lower workers’ compensation claims, healthcare costs, and lost productivity. Our analysis reveals these key benefits translate to significant financial savings over time.
Regulatory Compliance: Compliance with OSHA’s Bloodborne Pathogens standard is not only a legal requirement but also a demonstration of a healthcare facility’s commitment to employee safety. This can help avoid costly fines and penalties.
Enhanced Reputation: A healthcare facility with a strong reputation for safety and infection control is more likely to attract and retain both employees and patients. This can provide a competitive advantage in the marketplace.
Ethical Responsibility: Providing a safe and healthy work environment is an ethical responsibility of every employer. Implementing OPIM safety measures demonstrates a commitment to the well-being of healthcare workers.
Comprehensive Review of OPIM Safety Protocols
A comprehensive review of OPIM safety protocols reveals both strengths and weaknesses in current practices. While significant progress has been made in recent years, there is still room for improvement.
User Experience & Usability: From a practical standpoint, the usability of OPIM safety protocols depends heavily on the training and support provided to healthcare workers. When protocols are clear, concise, and easy to follow, healthcare workers are more likely to adhere to them consistently. In our experience with OPIM safety training, hands-on demonstrations and interactive sessions are the most effective.
Performance & Effectiveness: The effectiveness of OPIM safety protocols is directly related to their consistent implementation. When protocols are followed diligently, the risk of occupational exposure is significantly reduced. However, lapses in adherence can increase the risk of infection transmission.
Pros of OPIM Safety Protocols:
- Reduced Risk of Infection: As mentioned earlier, the primary advantage is the reduced risk of occupational exposure to bloodborne pathogens.
- Improved Employee Morale: Healthcare workers feel safer and more valued when OPIM safety protocols are in place.
- Enhanced Patient Safety: Minimizing the risk of infection transmission protects patients as well as healthcare workers.
- Regulatory Compliance: Compliance with OSHA’s Bloodborne Pathogens standard helps avoid fines and penalties.
- Cost Savings: Reducing the incidence of occupational exposures can lower healthcare costs and workers’ compensation claims.
Cons/Limitations of OPIM Safety Protocols:
- Cost of Implementation: Implementing OPIM safety protocols can require an initial investment in training, PPE, and safety-engineered devices.
- Complexity: Some OPIM safety protocols can be complex and difficult to understand, particularly for new healthcare workers.
- Human Error: Even with the best protocols in place, human error can still occur, leading to lapses in adherence.
- Resistance to Change: Some healthcare workers may resist adopting new OPIM safety protocols, particularly if they are perceived as time-consuming or inconvenient.
Ideal User Profile: OPIM safety protocols are essential for all healthcare workers who may be exposed to blood or other potentially infectious materials. This includes physicians, nurses, medical assistants, phlebotomists, laboratory technicians, and environmental services staff.
Key Alternatives: While there are no direct alternatives to OPIM safety protocols, some healthcare facilities may choose to implement more stringent infection control measures, such as enhanced cleaning and disinfection procedures or the use of advanced air filtration systems. However, these measures should be seen as complementary to, rather than replacements for, OPIM safety protocols.
Based on our detailed analysis, we recommend that all healthcare facilities prioritize the implementation of comprehensive and well-enforced OPIM safety protocols. This is essential for protecting the health and safety of healthcare workers and patients alike.
Navigating OPIM: A Summary of Best Practices
In conclusion, understanding the OPIM medical abbreviation and its implications is crucial for maintaining a safe and healthy healthcare environment. By implementing robust safety protocols, healthcare facilities can protect their employees from occupational exposure to bloodborne pathogens and other infectious agents. As leading experts in OPIM safety suggest, continuous training and adherence to best practices are paramount. We encourage you to share your experiences with implementing OPIM safety measures in the comments below and consult with your facility’s safety officer for specific guidance.
